Hello everyone!
It has been quiet on the blog for about 6 months, but we certainly haven’t been sitting still. On the contrary, a lot has happened and luckily, mostly good things. This blog post will mainly be informative to update everyone. In the end, it turned out to be 5 pieces of information, I could (or should) have written 5 different blog posts. At the same time, this is very indicative of life with a child that needs special care; it’s not that sometimes something is going on, something is ALWAYS going on – and often many things at the same time. So, once again, welcome to our world!
House
We moved! And even though we haven’t unpacked all of the boxes yet, we are very happy with the move. Our new house is exactly what we were hoping it would be: it’s more spacious, and Vera can get around easily with her walker and wheelchair, there is a changing station downstairs and she can use the front door she can use with her wheelchair without us having to lift her. There is a spacious bathroom and luckily, the house is also just a pleasant place to live. Lots of people showed up to help us with the move and we can’t thank everyone enough for lifting boxes, cooking, working on home improvement projects and just thinking of us in general. Both girls are getting settled nicely and so are we.
Heart
Prior to the move, at the beginning of summer, there was some concern regarding Vera’s heart. She was born with severe heart issues; a heart that beats very infrequently and at the same time at too high a frequency and can start racing. This was controlled fairly well with medication, although her heart was still beating too fast for her age. In the spring we found out that Vera acquired a new heart issue, not only does she have arrhythmia in the atrium, but now also in the ventricles. Which is even more dangerous, if the ventricles start racing, this could be life-threatening. This came as a shock. We practiced our resuscitation techniques again, just to be prepared. And we had a meeting with the cardiologist. The medication that will help with this is Flecainide. However, when Vera was only a few months old, her levels of this medication were too high and caused cardiac arrest. We were there when this happened at the intensive care in Amsterdam and we will never forget that moment. Luckily, she was in a place where immediate medical attention could be given and with resuscitation and medication, she narrowly made it. “Never again this medication” was always on her medication list in big, bold letters. But now, with the added issue of arrhythmia in her ventricles, we couldn’t just do nothing. And there was no alternative medicine. The cardiologist still felt it was the right course of action and the situation was different also now, 5 years later.
And so, in a very controlled way, we did end up starting with the Flecainide.
We started off with a very low dosage and made a weekly trip to the hospital for an EKG and blood draw to identify medication levels.
At home, we had a heart monitor to monitor her heart at night. And even though it was quite intrusive to have a heart monitor at home with all the beeps going on at night, it also gave us some reassurance. We dared to go to sleep because if something was really wrong, the alarm would sound and we could take immediate action. Each week we had one night where Vera was being cared for by a nurse (as always) so we could sleep for 8 uninterrupted hours knowing Vera was in good hands.
Over the course of the next couple of weeks, we gradually upped the medication levels. And, as is often the case with children who have Costello Syndrome, Vera needed quite a high dose to help alleviate the problem. But once this happened, it was good. Really good even. Her latest heart test showed no arrhythmia in the ventricles and her overall heart rate went down by 30 beats per minute.
This news almost sounded too good to be true. With the fear of the heart issues she had at birth and the cardiac arrest episode engrained in our memories, we could breathe a sigh of relief. Thank God! Her values have never been this good in her life.
This saves her body a lot of energy, beating 30 beats less in an hour means the heart isn’t working so hard and is beating 43,200 beats less in a day… We felt comfortable enough to get rid of the heart monitor and we will continue her semi-annual check-ups with the cardiologist. Because, even though her heart is functioning a lot better, it still isn’t functioning normally.
People often ask us if Vera can have heart surgery. The initial answer is that for now she is still too young and she doesn’t weigh enough yet, but hopefully: yes, maybe one day.
Vera’s heart nodes give off false impulses to the heart. When adults have this condition, a procedure can be done where the abnormal tissue that is causing the false pulses can be ablated (destroyed). Except Vera has so many false pulses that they can’t ablate all of it. But, who knows? Maybe one day this could be an option to get her heart to quiet down. But for now, this is not expected for the near future.
Eating
Before the summer, we also started eating therapy at school. Of course, essentially Vera has received eating therapy her whole life. From birth on (with the guidance of speech and language therapists who also specialize in swallowing difficulties) we have been practicing with bottles, spoons, licking and sipping.
Vera has always joined us at the table during meal times and we have always given her food to participate. And since birth, things have improved. Initially, she couldn’t bear any sensations around her mouth (except her pacifier), gradually she started touching food, holding food, licking food and putting food in her mouth. And eating a little bit. But definitely not enough yet and not the right kind of food to give her sustenance. And so, she has received her nutrition through a feeding tube for all of her life. First through her nose, later and to this day, through a mickey button in her stomach. 7 times a day we administer food or fluids or medicine through her mickey with a syringe.
At Vera’s school, there is the so-called EAT team, they support her language and speech therapist and us to help her learn to eat. What this means is that we essentially go back to baby food, porridge, and yogurt. Vera used to always spit this out. With eating therapy, she has started taking a spoonful of food in this little room at school and really eating it. Success! Fast forward to 6 months later and we’ve gone from the one spoonful to 2 fluid ounces. She now eats this every day. And we keep practicing with different foods, we give Vera anything she wants to try and will really eat. Even if that means it’s a cookie with whip cream. So that eating becomes a normal part of life and so Vera learns to get used to different tastes and textures. But it’s also about the technicalities: learning how to move the food from the front of the mouth to the back and actually going through the motions of swallowing it.
On the one hand, 2 fluid ounces seems a lot for her to eat by herself. On the other hand, this is still a far cry from being able to eat enough to really feed herself adequately.
We will still have to give it more time and patience, but she does seem to make progress.
Additionally, Vera also receives occupational therapy at school. Her eating issues are in large due to sensory sensitivities and occupational therapy helps with this. Vera’s body reacts to different stimuli in an overly sensitive way. Sound, touch and visual stimuli can be overwhelming for her. And that ties into how she deals with food. So, in therapy, she practices to get to know different sensations and not feel overwhelmed by them. In this way, playing with shaving cream with your hands contributes to learning to eat.
Sleeping
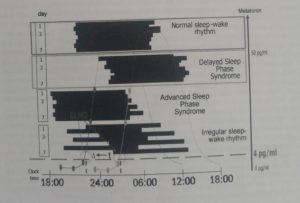
…or lack thereof. Another issue that Vera has had since birth. Vera is a restless sleeper and often wakes up crying at night and is done with sleeping at an early hour. We have already tried many things: Making her room darker, lighter, no noise or white noise in her bedroom, not too much food before bedtime or more food before bedtime, a nice bath and massage before bedtime, a weighted blanket, letting her cry longer or letting her cry shorter, making the room temperature warmer, colder, etc. She now takes sleep medication, which gives her two stretches of sleep a night, but still restless and interrupted. She never sleeps through the night. Needless to say, we are very tired often and Vera was getting headaches from lack of sleep. The neurologist referred us to the sleep clinic in Ede. They are specialized in sleep issues in patients with mental disabilities. It took some effort to get in (because who was going to pay for this?). And once we were in, they gave us quite a bit of homework. We filled out extensive questionnaires, kept a sleeping diary for 4 weeks, Vera slept with a machine that measures her movements at night for a week, and we took saliva samples that went to the lab to measure melatonin levels.
Sleep issues are difficult, not only because they make you very tired, but as parents, you feel so powerless that you can’t help your child fulfil this basic need. You start wondering what you are doing wrong and why it’s not going away. What’s going on? Is she in pain/is she hungry/is she scared? Or are we exaggerating and it’s not that bad?
The outcome of all the testing was quite illuminating. No sleep apnoea, no epileptic seizures. But we did find out that Vera’s body does not make any melatonin in the evening. She falls asleep because she is tired from the day, but not because her body gets sleepy. And that’s why she can’t stay asleep. The results from the movement monitor showed that she only really sleeps 54% of the time that she is in bed. When I heard that I felt so sorry for her. we go to her often at night, calm her down, tuck her in. And now it turns out that she is awake even more than we thought. And she must be so tired during the day.
So now we give Vera melatonin before bedtime, to replicate the natural process. We later found out that she doesn’t break down the melatonin during the day, which can also create issues with sleeping through the night. So, we switched her stomach medication to one that breaks down melatonin which she receives in the morning. For a while, it seemed we had found the solution. But, unfortunately, Vera’s sleeping pattern still varies and she continues to need sleep medication to even have a couple of stretches of sleep. The melatonin does give us hope, it feels like a step in the right direction. We are hoping it will lead to a more well-rested lifestyle for all of us.
Feet
Right around her 5th birthday, Vera was able to walk unassisted for a bit. She needed her custom shoes and a hula hoop for balance but was able to take small steps through the living room. Unfortunately, the positioning of her feet got worse after that, which made her less stable and walking became harder again. Thankfully, she did continue to walk well with her walker. It’s a common problem in children with Costello Syndrome; Vera has shortened calf muscles and her Achilles heel is too tight, which makes her walk on her toes, her heels were not touching the floor anymore. She also has splayed flat feet (sounds charming, doesn’t it?). The physiotherapy and orthopedic doctors referred us for casting. This means that every week, Vera’s feet are positioned as best as possible and then put in leg casts.
By the next week, her muscles and tendons are stretched a little bit and the process is repeated. We were not looking forward to this and were concerned it would impede her mobility or that it would be painful for her. But again, our little veteran is a trooper; she creates cheer for everyone in the casting room and she enjoys picking out a new color and glitter for her next casts. And at home and at school she is fully using her feet, she walks on the casts, does her physical exercises with her casts and accepts it fully. She only misses her nightly bath ritual and she is now heavier and clumsier for us to lift. She is currently in her 5th set of casts and we can see enormous improvement. Yay! We will continue this for a couple more weeks and after that Vera will get splints in custom shoes. This should help keep her feet in the correct position, so it doesn’t get worse again. And hopefully, she will walk better and better.
So in short
We are living in a great new house, with heart medication that is working well, we are busy eating baby food and are not quite sleeping at optimal levels and Vera keeps taking steps. Onwards we go!
Lots of love from all of us!
Some pics with her sister: