I cleaned out a large closet, which had everything to do with Vera.
Our girl is 10 years old now. And even though there are still concerns, there have also been some positive changes. And that’s why we’ve been able to get rid of some things.
Goodbye syringes, mickey buttons, extension hoses, metalline dressings, tubes of cream, freezer bins and liquid medications! For two years now, Vera has been eating everything independently. Every meal, snack and even her medication in pillform (which is about 10 pills a day). After 8 years of tubefeeding, I cannot tell you how special it is to watch her eat so well by herself these days. We take the fact that she develops some food related tics from time to time in stride. In particular when it comes to sandwich toppings, Vera will have a strong preference for one specific option for months. We’ve gone through phases of spreadable cheese, chocolate spread, cookiebutter and currently we’ve been in the hummus phase for months. All sandwiches have to have hummus, even in the morning at the breakfast table we’re surrounded by a strong garlic/chickpea aroma.
More things left the closet. Goodbye nebulizer, liquid medications for the nebulizer, plunger syringes! Eventhough Vera can still be plagued by common colds, in recent years she’s been able to get away with just regular nose sprays, perhaps one inhalerpuff and lots of rest. No more nebulizers or hospitalizations due to a cold. That used to be quite different in the past.
Goodbye diapers, wipes, endless diaper creams and goodbye changing station in the storage room. Another milestone we weren’t sure we were going to make (and neither did the urologist). Since 2021 Vera has been toilet trained during the day and since March of 2022 at night as well. What a difference this makes at home and out and about. And how nice for her skin that had been suffering from wearing diapers all these years.
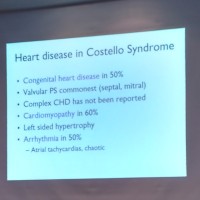
What remains is a container of medication for her heart and sensory processing during the night, a bottle of eardrops because ear infections are still a common occurence for Vera. What also remains is the cooler for growth hormones. Vera gets a dose of these every night.
The closet has been cleaned out.
The wheelchair stays, soon we’ll size up to a larger one again. The splints in her shoes also remain. Walking is still something for short distances as her legs and feet continue to be something we need to keep an eye on. We hope better splints will help. Or customized shoes, perhaps one day surgery. All in all this is probably the limit of Vera’s mobility. Her tricycle and the tandembike we like to take out to go shopping remain. What also remains are the hospital visits to see the pediatrician, endicrinologist, cardiologist, ENT doctor, eye doctor, oncologist, rehabilitation doctor. And in the background: the neurologist, orthopedist, urologist and dermatologist.
But what remains the most is a 10 year old schoolgirl who likes to be both handyman and princess, wants to dance and hang on the couch, makes us laugh and tires us out endlessly with her early rising, cognitive disabilities and a hint of autism.
But that’s Vera: our sister and daughter.
.
.