Report from the 2015 conference in Manchester: first part is generally (with some pictures), last part are details of the lectures (with some pictures of the presentations)
There was good atmosphere and it was educational, confrontational, busy and emotional…the Costello syndrome conference in Manchester was many things at once. First and foremost, it was once again special to meet other people with the syndrome. In The Netherlands we know 3 children besides Vera with Costello, being in the UK we could add 10 more with ages ranging between 2 and 30. All from different European countries. Because our children all look so similar and because we are dealing with such similar difficulties in our lives, these people quickly become family. We are able to have deep conversations quickly, where we share experiences and exchange tips. It instantly feels like we’ve known each other for much longer.
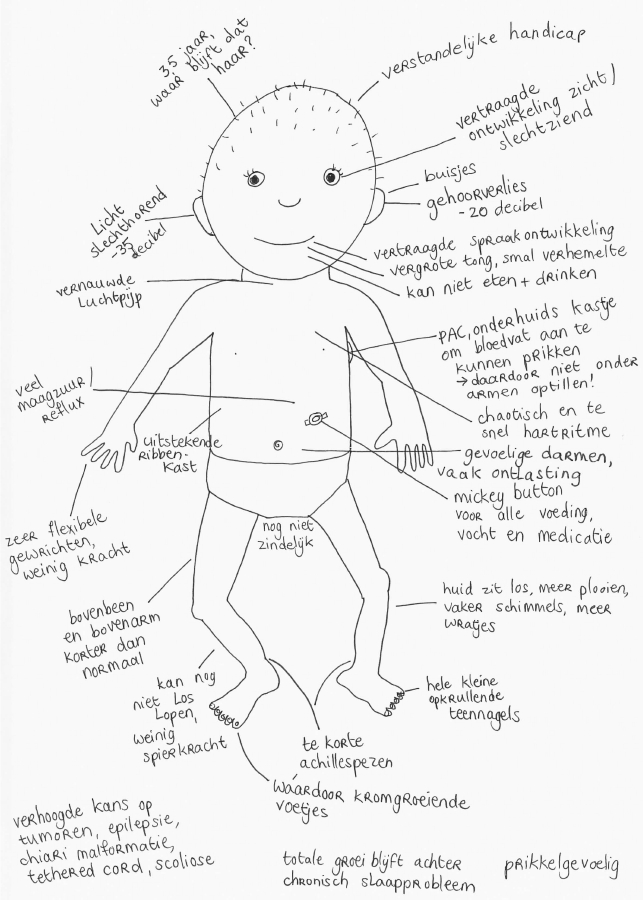
In some cases it gives us hope to see examples of what awaits Vera as she gets older and in other cases it can be quite confronting. Orthopaedic problems are fairly common, walking is possible for most people with the syndrome, but most use a wheelchair as well. Speech and language capabilities can vary greatly. And not everyone will be able to graduate from tube feedings. It became clear that, while the syndrome causes many similarities, every child or adult follows their own path with its own challenges, talents and limitations.
At this conference there were also about 20 families with children who have CFC, a syndrome that’s closely related to Costello. And again we had wonderful exchanges and saw many similarities, but also different challenges.
The days were planned so that there was time to spend time with the families, but also to attend lectures while there was a children’s program going on at the same time. Niels and I took turns attending lectures and spending time with the children. We’ve learned more about the increased chance of developing tumours, about autism and ADHD and the new knowledge about the decreased amount of growth hormones. We also heard about what was discussed during the American Costello conference in Seattle that took place earlier this year. We feel we moved up a notch again in our education about Vera and the Costello syndrome.
A direct effect of the information we gained during the conference is that we will look further into the shortage of growth hormones. Besides the fact that people with Costello syndrome tend to stay small, we now know that they have a shortage in growth hormones as well. This manifests itself not only in a completely different growth curve (Vera is now even deviating from the adapted CS growth curves), but also in impaired bone growth, less muscle mass, lack of energy and disrupted blood sugar levels.
We learned from two blood tests in the past that Vera’s levels of growth hormone are very low. Next week we will have a test to measure whether it truly is a shortage. If that is indeed the case, we are thinking of supplementing because it could improve her quality of life. This does mean she would need daily shots of growth hormone. We will wait for the test results and will consult with the endocrinologist to see what’s best for Vera.
And finally: a big thank you to our sponsors!
Thanks to you we were able to attend the European Costello conference in Manchester. We came back feeling enriched.
And with a suitcase full of fake spiders that have given me a fright on several occasions since then. (The spiders were from the Halloween party on the last night of the conference.)
= Details from the lectures for other parents, photos of presentations below =
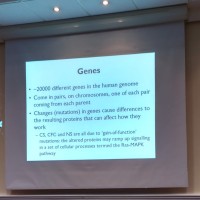
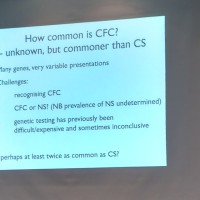
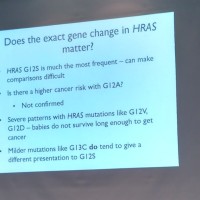
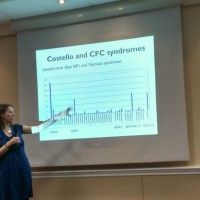
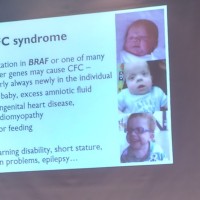
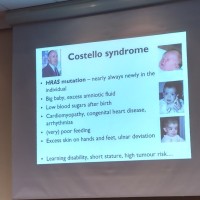
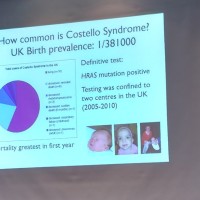
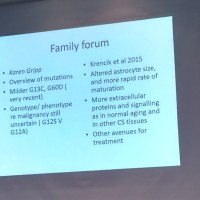
De first lecture was a general introduction by Dr. Emma Burkitt-Wright. She talked about genetics, in particular about the RAS-MAPK pathway and the differences between CS and CFC (since it was a joint conference) and how common these syndromes are estimated to be at this moment.
Things that stood out for me (Niels):
- a lot more attention is paid to low blood sugar levels in the US and the UK. (this has never been a big area of interest with Vera. Her blood sugar levels were checked recently but turned out not to be an issue for her. We have heard the same from other Dutch families).
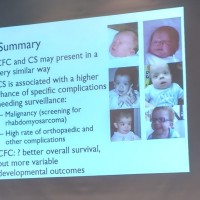
- It became clear that orthopaedic problems are of much greater concern with CS than with CFC.
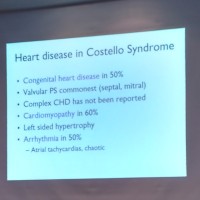
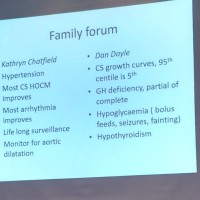
- The numbers associated with heart problems in people with CS (see photo of sheet) are impressively high, in particular the enlarged heart muscle (cardiomyopathy) in 60% of CS cases.
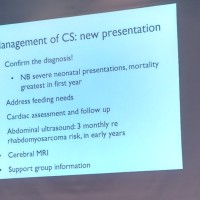
- For further monitoring of the complications of CS it was recommended to have ultrasounds done 4 times a year to catch possible tumours at an early stage. This has been done with Vera as well. It was recommended to keep doing this at this frequency until the age of 7 after which the testing could be done less often.
- A head MRI was also recommended, possibly to detect chiari malformation. We suspect Vera will get this MRI in the coming weeks.
- And finally the importance of a support group for parents was emphasized (a lot of valuable information gets exchanged there, information doctors may not have direct access to or information about which nothing has been published yet), we can only confirm this!
The second lecture was given by Dr. Bronwyn Kerr, an authority in the field of CS research. She gave us an overview of what was discussed at the CS symposium in Seattle earlier this year. What we learned from the Seattle overview:
- heart monitoring should be life long, the frequency can be lowered as the person gets older.
- there are adapted growth curves for CS, if growth deviates from these curves, testing is recommended to determine growth hormone levels present in the blood. Supplementing with growth hormone is only beneficial if there is a shortage, which is then only supplemented until normal levels are reached.
- the topic of hypoglycaemia when giving several tube feedings a day was brought up
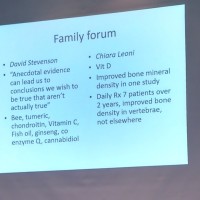
- she talked about nutrition and the lack of causal effect between vitamin C, fish oil, ginseng, co-enzyme Q etc. and improvement (more research was needed for further evidence, it can be hard to determine which factor contributed to improvement).
- improvement of bone density with vitamin D: research has been started to determine the relationship, early outcomes have been varying.
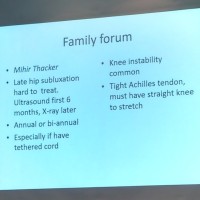
- hips: it was recommended to check the hips periodically (annually or twice a year through x-ray, during the first months it can still be done with ultrasound) in particular if tethered cord is present. Instability of the knee is a known fact and should also be checked by the paediatrician (being able to stretch the knee fully).
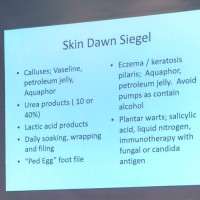
- skin problems were discussed as well; this doesn’t apply to us yet, but useful tips on the sheets about the use of alcohol free products to make sure the skin doesn’t dry out further (in particular with shoes).
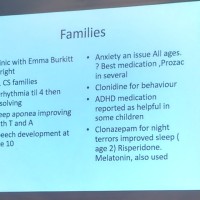
- from family surveys in Seattle we learned that arrhythmia often improves after age 4 and speech improves after age 10.
- anxiety disorder is present in many children, some benefit from the use of the medicine Prozac.
- for behavioural problems the medication Clonidine is often used. Or medication that is often prescribed for ADHD.
- sleep problems are a common issue that occur often in many and for long periods of time. Several types of medication are being used, the early years are the hardest. This is an issue that deserves more research as it has a huge impact on the lives of parents and children and is a heavy burden.
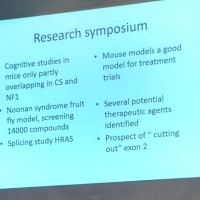
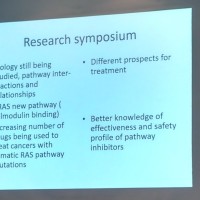
- several studies are currently being done with a mouse with characteristics of CS and NF1 (important to test treatment and influence of signals in the cells), for Noonan syndrome there is a fruit fly model (a lot of information about treatment and how the cells react was gained from this, because it could be repeated quickly and often).
- there are important developments in the HRAS splicing study (and removing exon2). I do not have sufficient DNA knowledge to expand on this.
The next lecture was by Dr. Peter Clayton about growth differences and treatment. In short (by Leonie): people who are affected by CFC and CS have small stature as a result of their genetic makeup. Decreased amounts of growth hormone can also be present. Dr. Clayton advocated to supplement with growth hormones, if this was the case, until normal levels are reached. Not necessarily to gain height, but to improve quality of life in the first place. Growth hormones regulate growth, blood sugar levels, bone growth and muscle mass. With CS there is often fear that growth hormones would also increase the chance of developing tumour cells (with an already increased chance of cancer). No evidence of this has been found. The thickening of the heart muscle does deserve special attention, however.
Dr. Shruti Garg did a study in the UK on behavioural problems in children with CFC and CS. The last lecture I attended was about this. Behavioural problems appear to be fairly common. The large majority shows signs of AD(H)D and autism. Dr. Garg stated that it could be very beneficial to seek a separate diagnosis. Often, the behaviour is grouped under the characteristics of the syndrome. If a separate diagnosis is attained, more concrete treatment can take place with behavioural therapy and/or medication.